- A Zenker’s diverticulum (ZD) is a type of esophageal diverticulum that is a common cause of dysphagia in the elderly.
- Broadly speaking, esophageal diverticula can be classified by their location, their degree of involvement of the lumen (true or false), and their mechanism of origin (traction or pulsion).
- Location:
- Pharyngoesophageal
- Midesophageal
- Epiphrenic.
- True or false:
- True diverticulum: A true diverticulum involves all layers of a luminal wall, such as with a Meckel’s diverticulum.
- False diverticulum: A false diverticulum only involves some of the layers of a luminal wall, such as with a Zenker’s diverticulum (which involves the mucosa and submucosa only).
- Traction or pulsion:
- Traction diverticulum: caused by pulling forces external to the structure. For instance, there may be pulling forces on the esophagus from hardware after cervical spinal surgery.
- Pulsion diverticulum: due to pushing forces from within a structure.
- A Zenker’s diverticulum is considered a pharyngoesophageal, pulsion, false diverticulum as above.
Epidemiology
- Zenker’s diverticula are one of the most common types of esophageal diverticula with an annual incidence of 2 per 100,000 people.
- There is a 2-3:1 male to female preponderance.
- The typical age of presentation is in the 7th to 8th decades of life.
Pathophysiology
- With a Zenker’s diverticulum, increased intraluminal pressure is thought to arise due to problems with complete relaxation or opening of the cricopharyngeus.
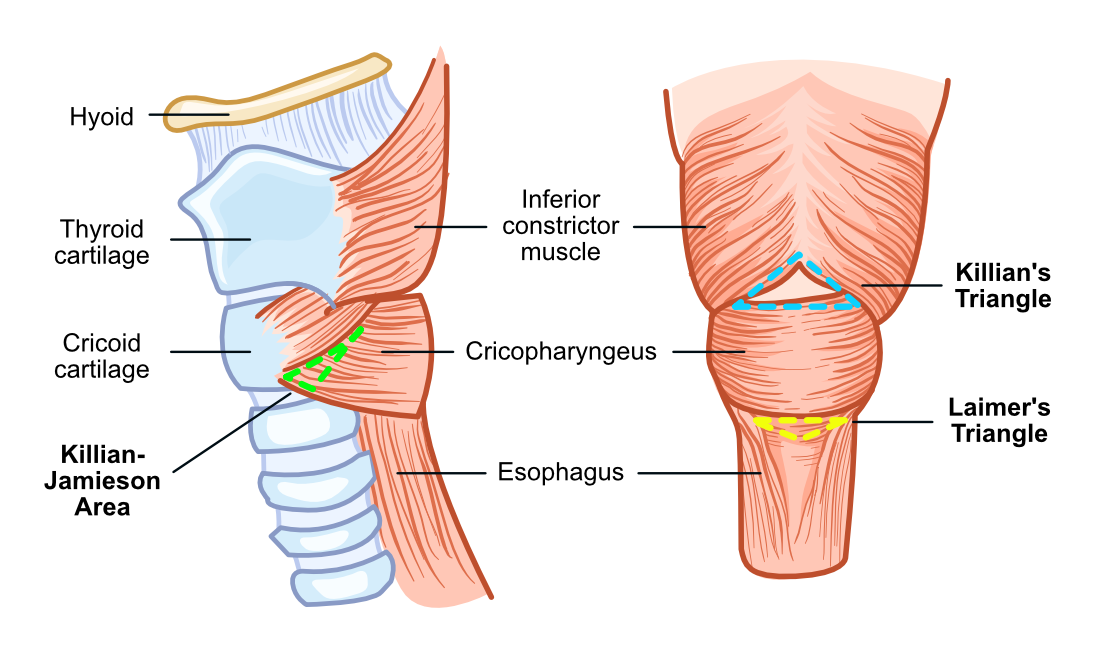
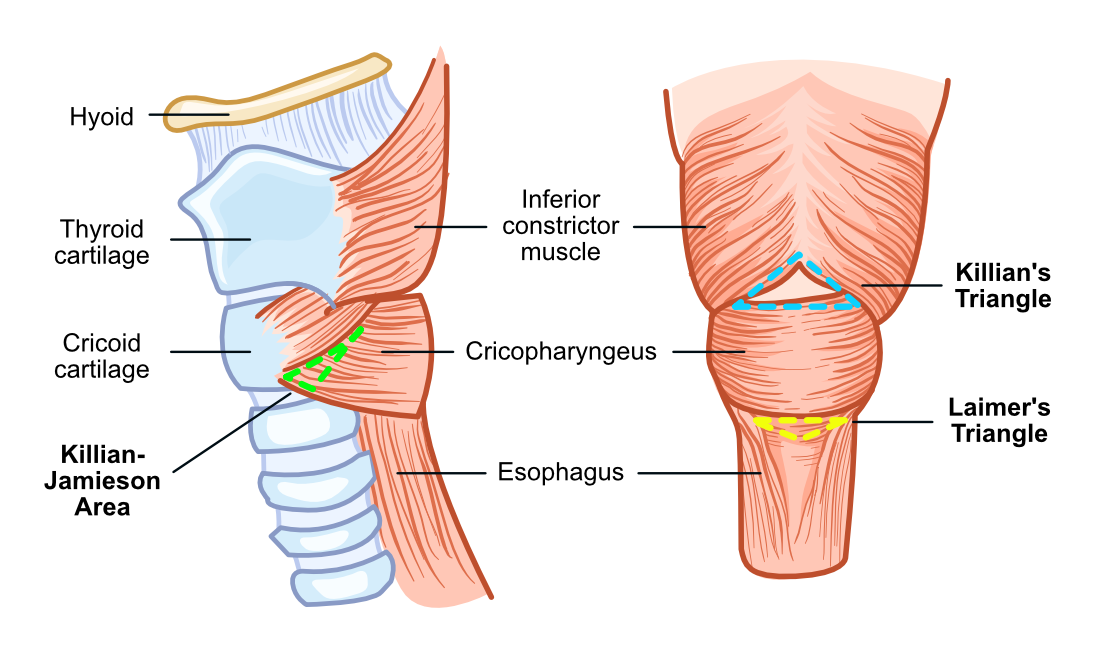
- This increased pulsion pressure results in herniation of the esophageal mucosa and submucosa through an area of weakness called Killian’s Triangle.
- Boundaries of Killian’s triangle:
- Superior: inferior constrictor
- Inferior: cricopharyngeus
- Zenker’s diverticula are more common on the left than on the right. This is thought to be because the carotid artery is more lateral on the left side, and because the esophagus has a slight convexity towards the left.
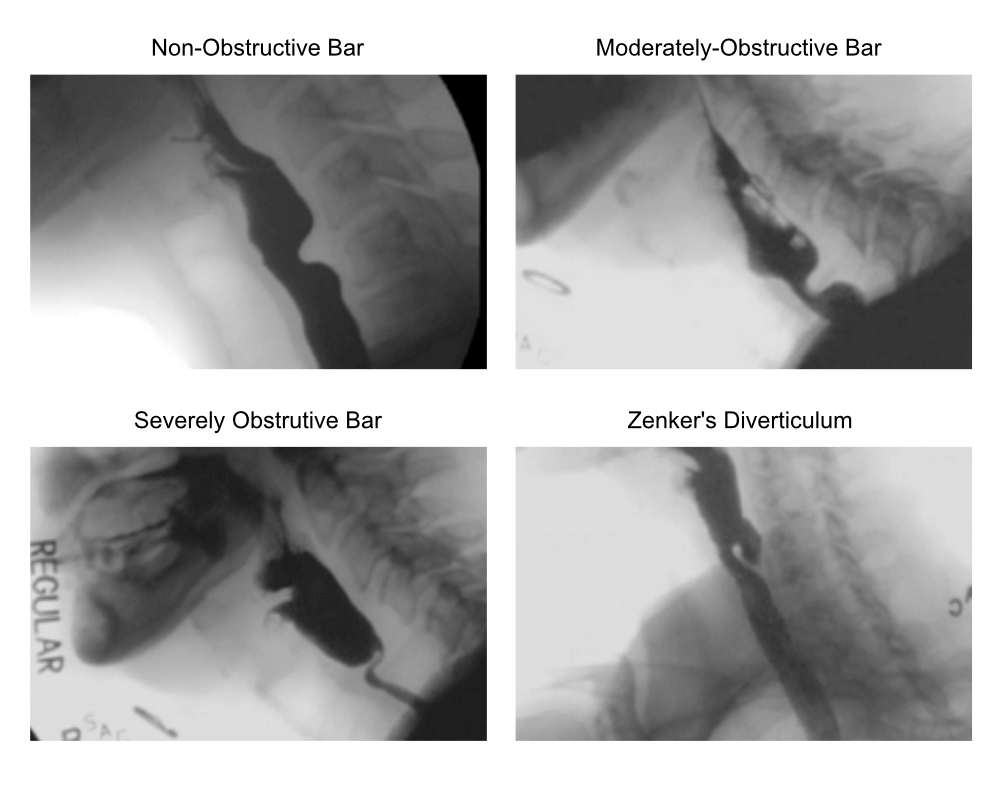
- The failure of coordinated relaxation or expansion of the cricopharyngeus is called cricopharyngeus muscle dysfunction (CPD), which can be viewed as a gradient of disease that can eventually give rise to a Zenker’s diverticulum.
- Progression of cricopharyngeus muscle dysfunction:
- Non-obstructive bar (NOB): no impediment to bolus flow
- Moderately-obstructive bar (MOB): occupies up to half of the upper esophageal sphincter (UES) lumen.
- Severely obstructive bar (SOB): near complete UES narrowing.
- Zenker’s diverticulum (ZD)
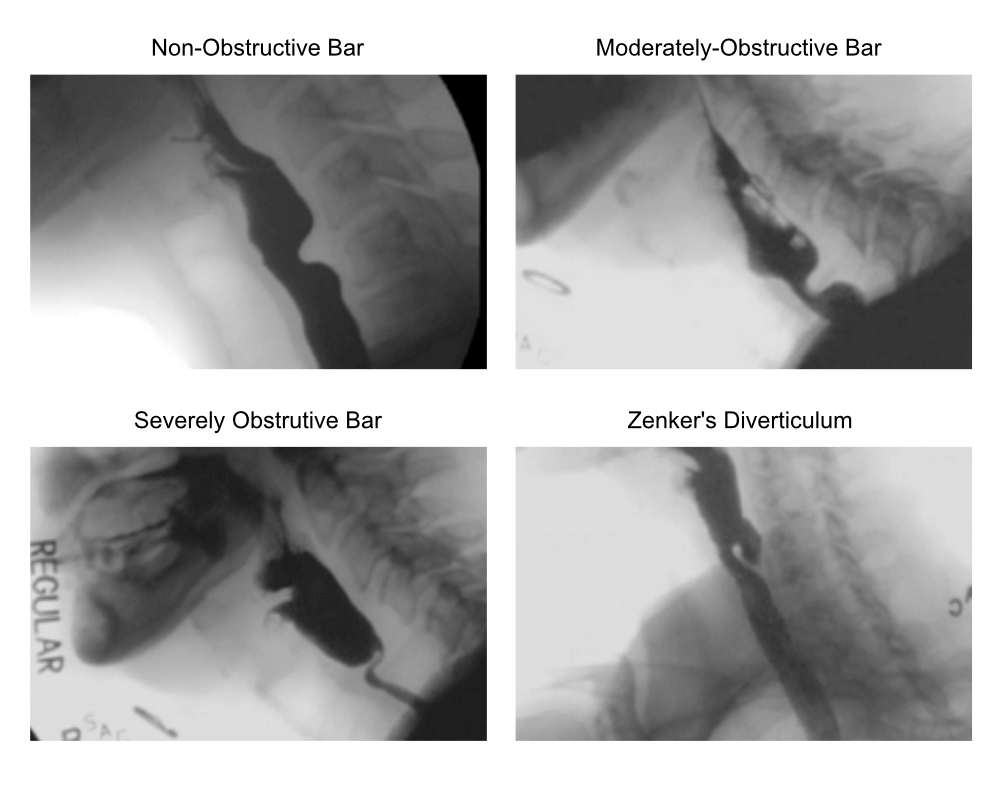
Cricopharyngeus muscle dysfunction. Adapted from Randall et al: "Improved symptomatic, functional, and fluoroscopic outcomes following serial “series of three” double-balloon dilation for cricopharyngeus muscle dysfunction."
Signs and Symptoms
History
- The predominant symptom in patients with a Zenker’s diverticulum is progressive dysphagia.
- Other symptoms that may present include delayed regurgitation of partially digested meals, choking, coughing, globus, weight loss, and recurrent aspiration pneumonia.
- Gurgling with deglutition (also known aso known as borborygmi) can sometimes be present as well.
Physical Examination
- Physical examination is usually non-contributory in patients with a Zenker’s diverticulum.
- Flexible nasolaryngoscopy may show pooling of mucous in the hypopharynx but is typically normal.
- In rare cases, there may be a Boyce’s sign – a swelling in the neck that gurgles on palpation.
Diagnosis
- Barium swallow: mainstay of diagnosis.
- Esophagogastroduodenoscopy (EGD): may identify an incidental ZD in patients undergoing gastrointestinal evaluation for other reasons.
Treatment
- Treatment of a Zenker’s diverticulum depends on the presence or absence of symptoms. In patients with symptoms, treatment is primarily surgical.
- In patients with cricopharyngeal muscle dysfunction and a cricopharyngeal bar, esophageal dilatation or botulinum toxin injection into the cricopharyngeus can be used as a sole treatment or adjunctive option.
- Surgical options can be divided into open procedures and endoscopic procedures.
- Generally speaking, endoscopic procedures have lower associated morbidity but higher recurrence rates.
Endoscopic Procedures
- Endoscopic Diverticulotomy
- Visualization of the Zenker’s diverticulum is obtained transorally and the common wall between the diverticulum and esophagus is divided.
- Division of the common wall is done with electrocautery, CO2 laser, or with a stapler.
- Modified Transoral Resection of Diverticulum (MTORD)
- One potential disadvantage of an endoscopic diverticulotomy is a higher recurrence rate due to incomplete resection of the cricopharyngeus and a remnant diverticulum.
- To address these limitations, a modified transoral resection of diverticulum (MTORD) technique has been described.
- This technique involves visualization of the common wall as with an endoscopic diverticulotomy, but then also includes elevation of a mucosal flap, complete muscle resection, and excision of redundant mucosal tissue.
Open Procedures
- Cricopharyngeal myotomy
- This can be done as a sole procedure in patients with a small Zenker’s diverticulum, but is more commonly done in combination with the techniques described below.
- Here the fibres of the cricopharyngeus are identified and divided via a transcervical approach. Care is taken to avoid esophageal mucosal violation.
- External diverticulectomy
- Rigid esophagoscopy is first performed and the Zenker’s diverticulum is packed to facilitate its identification externally.
- A transcervical approach is performed and the diverticulum is truncated at its base, typically with a stapler.
- Because the esophageal mucosa is violated, a feeding tube is inserted and enteral nutrition is maintained for a few days post-operatively.
- Inversion technique
- In this technique, following a cricopharyngeal myotomy, a purse string suture is loosely tied around the neck of the diverticulum.
- The diverticulum is then inverted into the esophagus and the purse string is pulled tight and is oversewn.
- Because the esophageal mucosa is not violated, enteral nutrition is not required. However, the diverticulum itself is not excised.
- Diverticulopexy
- With a diverticulopexy, following a cricopharyngeal myotomy, the diverticulum is mobilized and then tacked superiorly to the prevertebral fascia to eliminate the false pocket.
- This has similar advantages and disadvantages to an inversion technique.
Last updated December 20, 2022