| T Category |
Criteria |
| TX |
Primary tumour cannot be assessed
|
| Tis |
Carcinoma in situ.
|
| T1 |
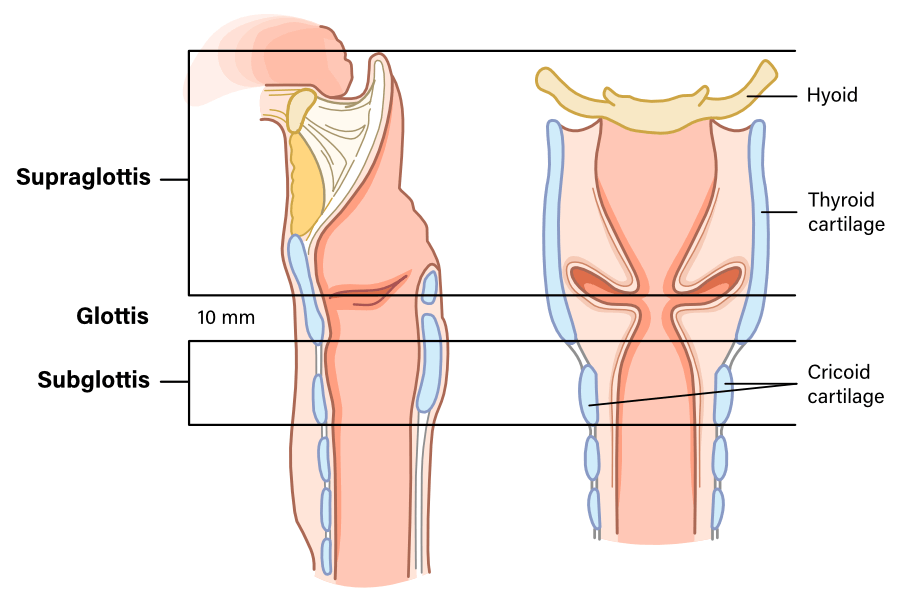
Tumour limited to 1 subsite of the supraglottis only and with normal vocal fold mobility.
|
| T2 |
- Tumour involves more than 1 subsite of the supraglottis OR has glottic extension OR has hypopharyngeal or oropharyngeal mucosal extension. (eg. mucosa of base of tongue, vallecula, medial wall of pyriform sinus).
- AND without vocal fold fixation.
|
| T3 |
- Vocal fold fixation.
- OR invades any of the following: postcricoid area, preepiglottic space, paraglottic space, and/or inner cortex of thyroid cartilage.
- OR extension to the mucosa of the esophagus.
|
| T4a |
- Moderately advanced local disease
- Tumor invades through the outer cortex of the thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, esophagus, soft tissues of neck, thyroid, extralaryngeal strap muscles.).
|
| T4b |
- Very advanced local disease
- Tumour invasion of the prevertebral fascia, carotid artery encasement, or involves mediastinal structures.
|
| T Category |
Criteria |
| TX |
Primary tumour cannot be assessed
|
| Tis |
Carcinoma in situ.
|
| T1a |
Tumour limited to one vocal fold only.
|
| T1b |
Tumour involves both vocal folds (eg. involving the anterior commissure).
|
| T2 |
- Tumour extends into the supraglottis or subglottis.
- OR vocal fold paresis.
|
| T3 |
- Vocal fold fixation.
- OR invasion of the paraglottic space, and/or inner cortex of thyroid cartilage.
|
| T4a |
- Moderately advanced local disease
- Tumor invades through the outer cortex of the thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, esophagus, soft tissues of neck, thyroid, extralaryngeal strap muscles.).
|
| T4b |
- Very advanced local disease
- Tumour invasion of the prevertebral fascia, carotid artery encasement, or involves mediastinal structures.
|
| T Category |
Criteria |
| TX |
Primary tumour cannot be assessed
|
| Tis |
Carcinoma in situ.
|
| T1 |
Tumour is limited to the subglottis.
|
| T2 |
- Tumour extends into the glottis.
- OR vocal fold paresis.
|
| T3 |
- Vocal fold fixation.
- OR invasion of the paraglottic space, and/or inner cortex of thyroid cartilage.
|
| T4a |
- Moderately advanced local disease
- Tumor invades through the thyroid or cricoid and/or invades tissues beyond the larynx (e.g., trachea, esophagus, soft tissues of neck, thyroid, extralaryngeal strap muscles.).
|
| T4b |
- Very advanced local disease
- Tumour invasion of the prevertebral fascia, carotid artery encasement, or involves mediastinal structures.
|