| T Category |
Criteria |
| TX |
Primary tumour cannot be assessed
|
| Tis |
Carcinoma in situ.
|
| T1 |
- Tumour 2 cm or smaller in greatest dimension.</span>
- AND DOI ≤ 5 mm
|
| T2 |
- Tumour > 2 and ≤ 4 cm in greatest dimension with
DOI ≤ 10 mm
- OR tumour 2 cm or smaller in greatest dimension with DOI > 5 mm but ≤ 10 mm.
|
| T3 |
- Tumour > 2cm and ≤ 4cm with DOI > 10 mm
- OR tumour > 4 cm with DOI ≤ 10 mm
|
| T4a |
- Tumour > 4 cm AND DOI > 10 mm
- OR tumour invasion of adjacent structures only (including through cortical bone of the mandible or maxilla, or involves the maxillary sinus or skin of the face).
- Note that superficial erosion of a bone/tooth socket (alone) by a gingival primary is not sufficient to classify a tumor as T4.
|
| T4b |
- Very advanced local disease
- Tumour invasion of the masticator space, pterygoid plates, skull base, or encasement of the internal carotid.
|
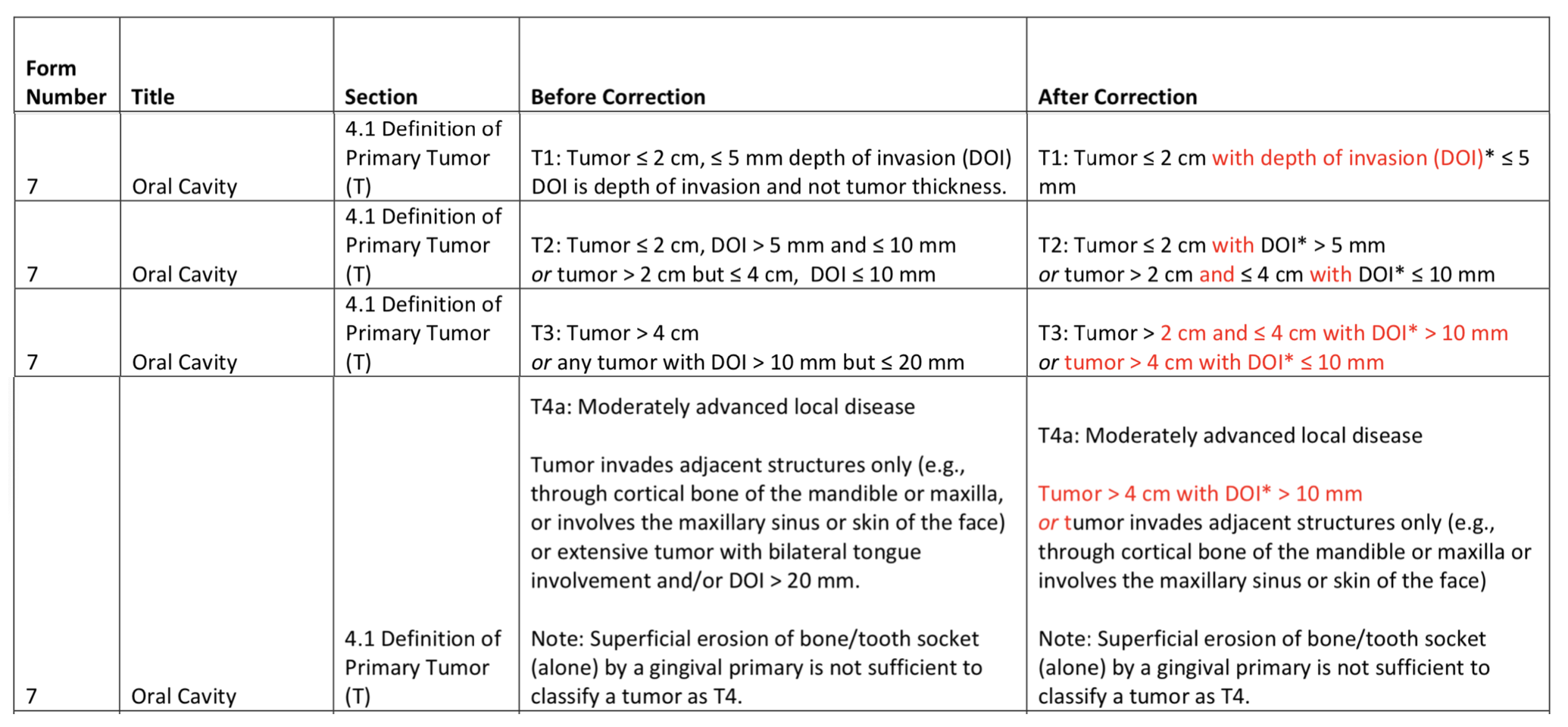
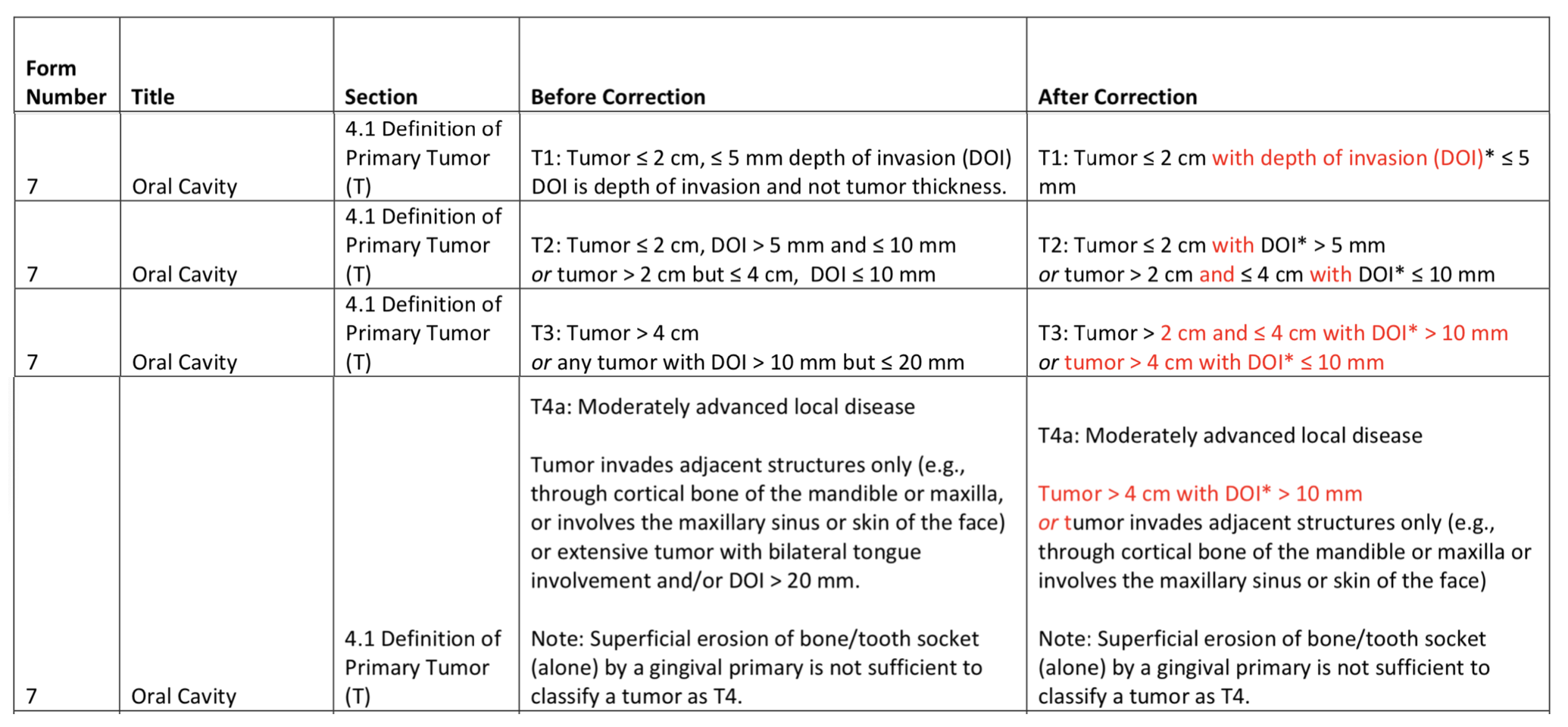
General Rules
- Previously, T1, T2, and T3 were defined only by tumour size (≤2 cm, >2 - 4 cm, and >4 cm respectively). Now depth of invasion (≤5 mm, >5 - 10 mm, and >10 mm) plays a role as well.
- To be considered T1 you must have a tumour size ≤ 2 cm AND a DOI ≤ 5 mm.
- Increasing DOI essentially increases your T categorization by 1. For instance, if you have a ≤2 cm tumour but your DOI is 5-10 mm, then this is T2 not T1. If you have a a >2 - 4 cm tumour but your DOI is >10 mm then this is T3 and not T2. If you have a >4 cm tumour but your DOI is >10 mm then this is T4a and not T3.
- Many online sources will contradict this because the 8th Edition had multiple revisions which significantly changed oral cavity staging. Not only do they not exclude the dry (vermillion) lip, but the definitions for T2/T3/T4a have changed as well compared to the initial release of the 8th Edition. See published changes below:
Changes in the 8th Edition 3rd Printing
AJCC 8th Edition Supplement
Depth of Invasion versus Tumour Thickness
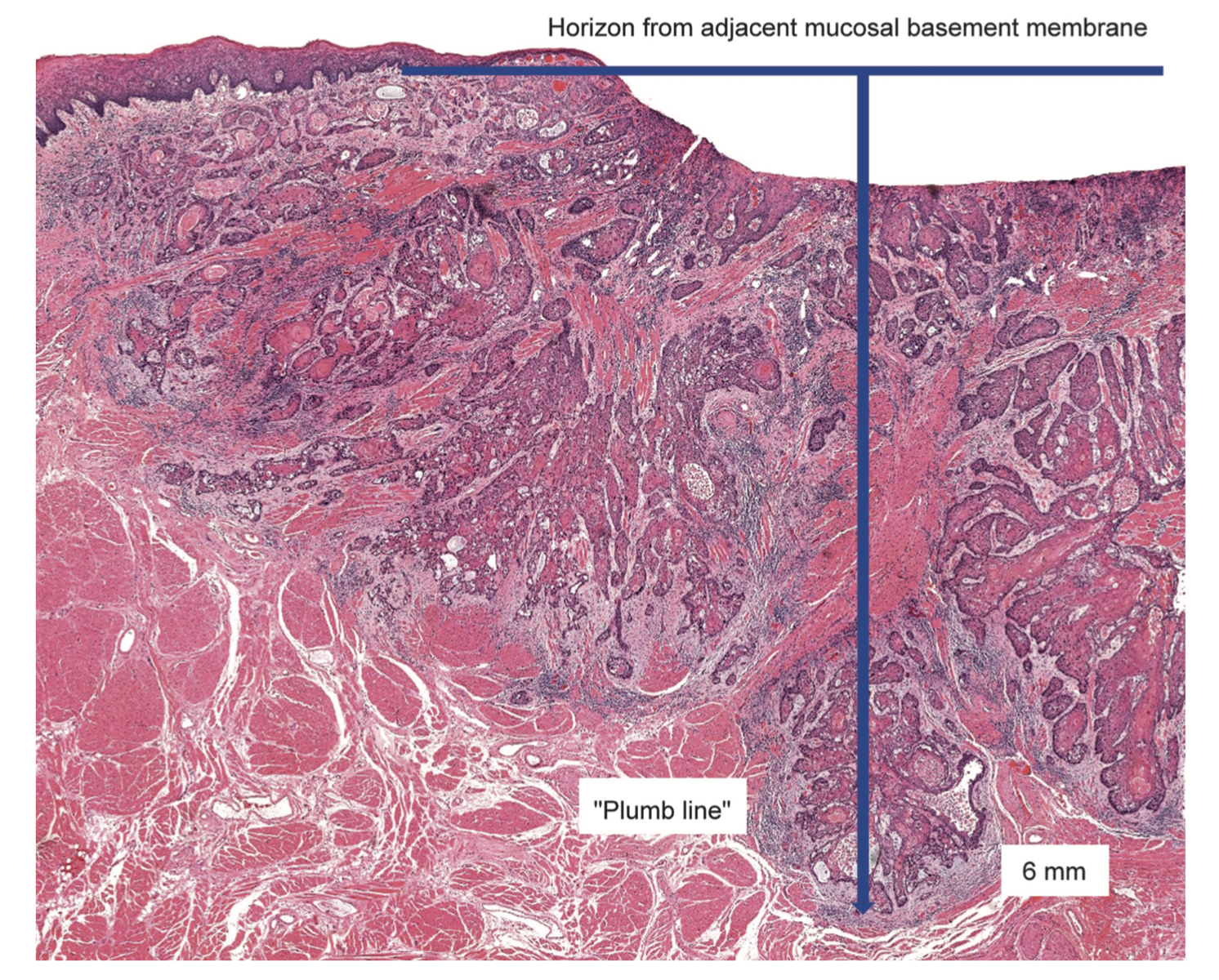
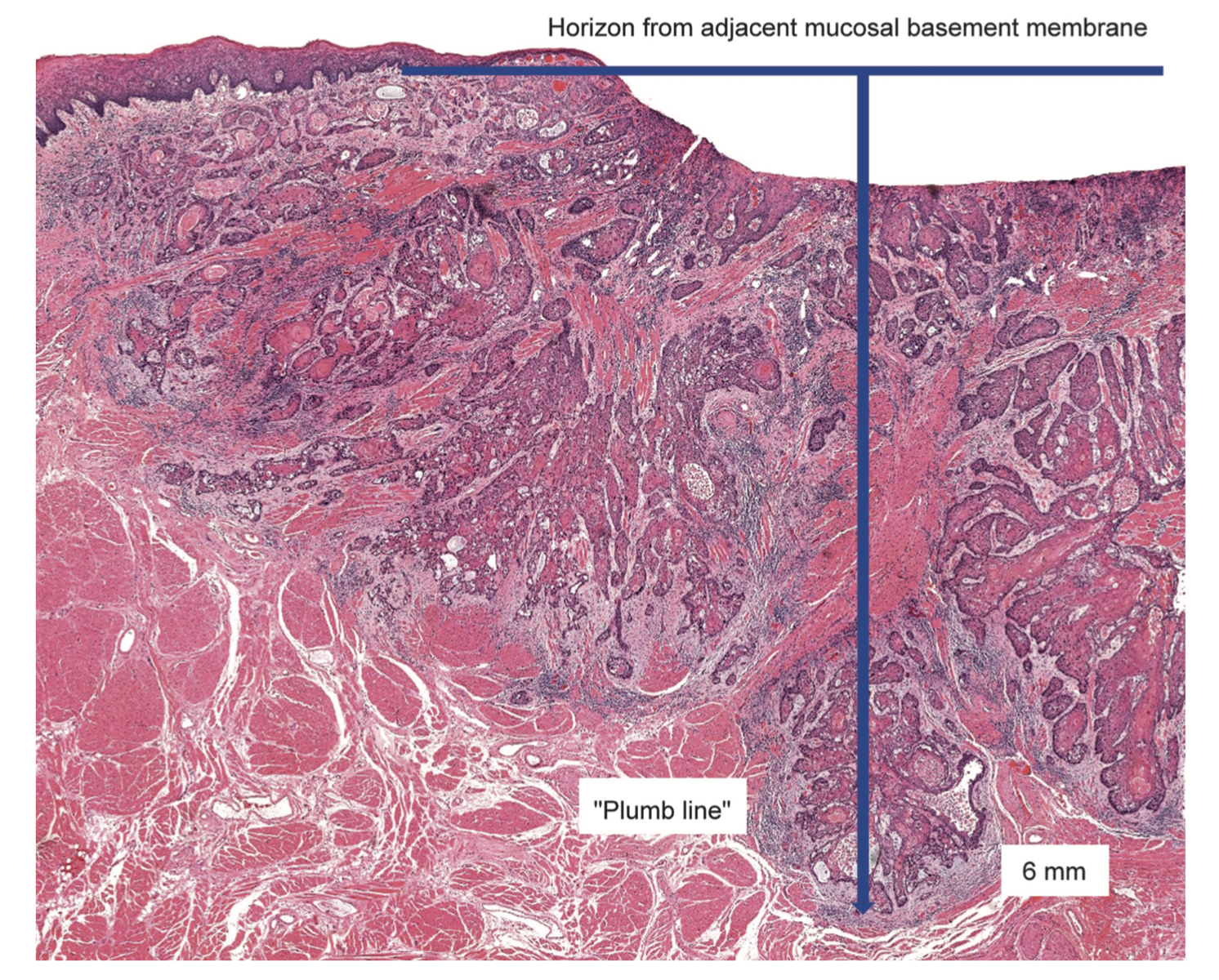
- Depth of Invasion (DOI) is not the same as tumour thickness.
- Tumour thickness measures the distance from the most superficial to the deepest aspect of the tumour.
- Depth of invasion is calculated by measuring the distance to the deepest aspect of the tumour measured from a line parallel to the basement membrane of the nearest intact squamous mucosa.
- A plumb line is drawn from the 'horizon' from the nearest intact basement membrane and is used to measure the DOI.
- If a tumour is very exophytic, the tumour thickness will be greater than the depth of invasion. Conversely, if a tumour is very ulcerated, the depth of invasion may be greater than the tumour thickness (as seen in the example below).